What is Penile Hypospadias? Unraveling the Mystery
The Anatomy of Hypospadias: Understanding the Condition
Penile hypospadias is a congenital medical condition characterized by an abnormal location of the urethral opening on the penis. In a typical male anatomy, the urethra opens at the tip of the glans penis, allowing for the normal emission of urine and semen. However, in cases of hypospadias, this opening can occur anywhere along the shaft of the penis, or even at the perineum, the area between the scrotum and the anus. This malformation arises during fetal development, as the urethra fails to form properly, leading to various physical and functional issues.
The severity of hypospadias varies and can significantly affect both the function and aesthetic appearance of the male genitalia. Beyond the physical implications, understanding this condition requires awareness of the anatomical complexities involved. The condition can coincide with other genital anomalies and can influence subsequent reproductive health if left untreated. Thus, a comprehensive exploration of hypospadias is imperative for both affected individuals and their families.
Types of Hypospadias: From Mild to Severe
Hypospadias is categorized into several types based on the location of the urethral opening. The three primary classifications include:
- Glanular Hypospadias: The opening is located at or near the glans penis. This is the least severe form and often can be treated with minor surgical adjustments.
- Coronal Hypospadias: The urethral opening is situated at the corona, the ridge of the glans. While this implies more functional issues than glenoid cases, many children can achieve satisfactory results with surgical intervention.
- Shaft Hypospadias: The opening is further down the shaft of the penis, leading to more significant complications. This type is often more challenging to treat and can have a pronounced impact on urinary function and sexual health in adulthood.
In its most severe manifestation, known as panhypertrophy, the urethra may open at the perineum or have an associated chordee (curvature of the penis), which presents additional challenges for surgical correction and aesthetic restoration. Understanding these distinctions is vital in developing treatment plans and managing expectations for patients and their families.
Causes and Risk Factors: What You Need to Know
The exact causes of hypospadias remain largely undetermined, but several risk factors have been identified through research and clinical observations. While genetic components play a crucial role, environmental factors also significantly contribute to the condition’s occurrence.
One of the most influential factors appears to be maternal health during pregnancy. For example, maternal exposure to certain medications (especially hormonal treatments), smoking, and advanced maternal age can increase the risk of a male child being born with hypospadias. Additionally, a family history of the condition can suggest a genetic predisposition; hypospadias is often observed to run in families, indicating that inherited traits may influence urethral development.
It is essential to raise awareness and educate parents about these potential risk factors, especially for those planning for parenthood, as understanding these can inform decisions about prenatal care and overall health management throughout pregnancy.
Diagnosis: How Is Penile Hypospadias Detected?
The Role of Pediatric Urologists: Experts at Work
Diagnosis of penile hypospadias typically occurs shortly after birth, often during routine examinations by pediatricians or obstetricians. However, specialized assessments by pediatric urologists become crucial for evaluating the extent and particularities of the condition. These specialists possess the expertise to not only diagnose the condition but also develop an effective treatment plan tailored to the individual needs of the child.
During clinical assessments, the urologist will conduct a thorough genital examination to determine the degree of hypospadias and assess for any associated anomalies such as chordee or undescended testicles. Their extensive background enables them to foresee possible complications and engage in informed discussions with parents about the implications of the diagnosis and the recommended treatment approaches.
Diagnosis Techniques: From Physical Exams to Imaging
While physical examination is often sufficient for diagnosing hypospadias, further imaging techniques may be employed in certain cases to assess associated anomalies or to prepare for potential surgical interventions. Ultrasound imaging techniques can provide valuable information regarding the location of the urethra and any concurrent malformations within the male genitalia. Additionally, sophisticated imaging modalities, such as MRI, may occasionally be utilized for further investigation, especially in cases that complicate surgical planning due to co-existing anatomical variations.
Ultimately, the diagnosed severity of hypospadias and any associated anatomical issues provide critical information that guides surgical and therapeutic pathways, emphasizing the importance of an accurate and comprehensive examination process.
What Parents Should Look For: Early Signs and Symptoms
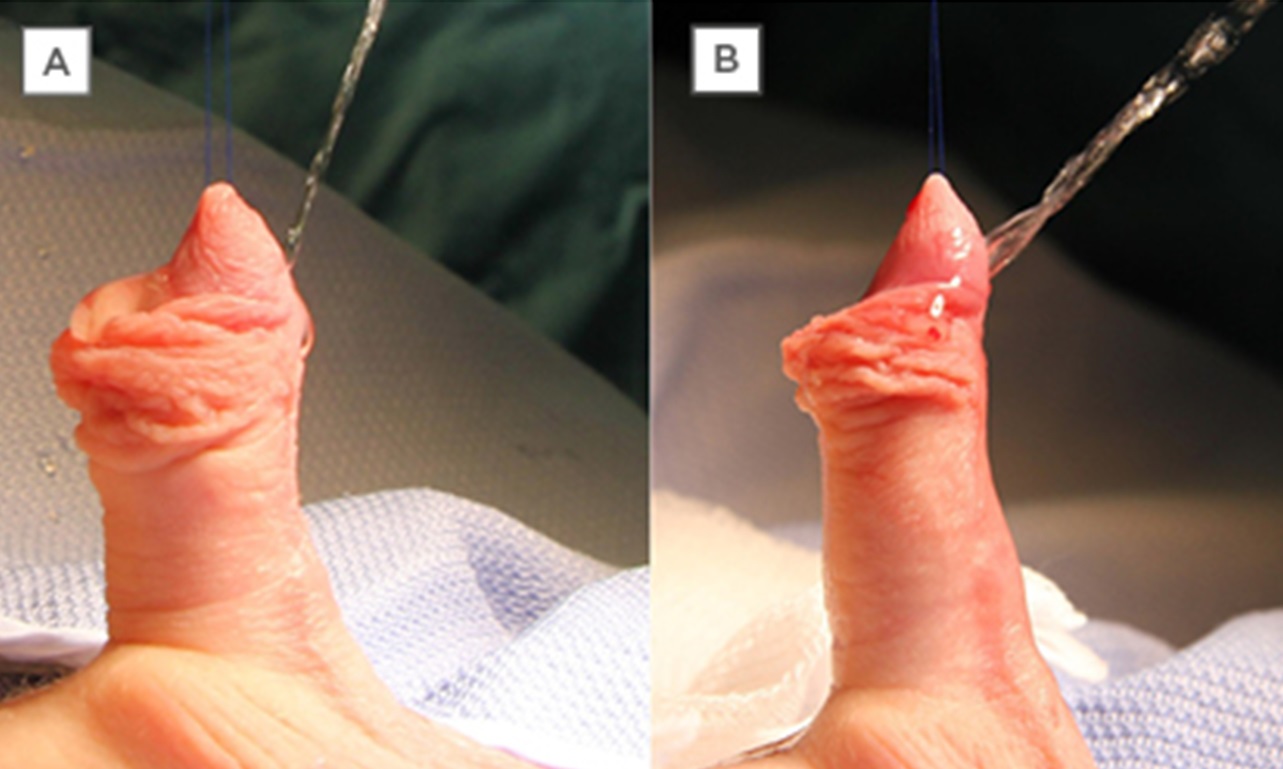
Awareness is key for parents in recognizing the potential signs of hypospadias. In the newborn period, parents can often notice abnormalities in the external genitalia during routine care and diaper changes. Specific indicators may include a urethral opening that is not located at the tip of the penis, abnormal curvature, or a divided glans. Additionally, the appearance of a noticeable penile deformity or disproportion can raise concerns about possible hypospadias.
Parents should be attentive to issues related to urination, such as difficulties in establishing a strong urinary stream, abnormal positioning during urination (e.g., sitting instead of standing), and signs of urinary tract infections, which could indicate an underlying anatomical disorder. Early detection is paramount; therefore, frequent evaluations during those critical first weeks of life could lead to prompt diagnosis and better long-term outcomes.
Treatment Options: Navigating the Road to Recovery
Surgical Interventions: When and Why They Are Necessary
Surgical treatment is often the primary recommendation for hypospadias to correct the position of the urethral opening and restore normal penile function. The timing for surgery is generally considered optimal between 6 to 18 months of age, allowing for growth and development while addressing functional needs.
There are several techniques employed during corrective surgery; the method chosen typically depends on the severity and type of hypospadias diagnosed. Tunica vaginalis flap, Mathieu repair, and the use of grafts from the skin are common surgical procedures utilized based on the individual anatomical situation. The main goals include ensuring a normal urinary function, aesthetically reconstructing the penis, and preventing potential complications in adulthood, such as sexual dysfunction or psychological distress.
It is important to communicate with parents regarding the expected outcomes, potential complications, and the necessity for follow-up evaluations to monitor postoperative healing and compliance with any ongoing treatment regimens.
Non-Surgical Approaches: Understanding the Alternatives
In some mild cases of hypospadias, especially glanular types, non-surgical management may be an option. Conservative approaches may include careful observation, effective parental education about hygiene, and regular monitoring of urinary patterns and any potential complications that may arise due to the condition. Using topical agents and preservation of proper genital health can promote optimal conditions and delay surgical intervention.
However, it is essential for healthcare providers and families to continuously assess this decision, as the risks of delaying surgery may become more pronounced. As the child approaches school age, psychological aspects relating to appearance and function may prompt families to reconsider the need for surgical correction, indicating that ongoing dialogue with urologists and mental health professionals is critical.
Postoperative Care: Ensuring Optimal Healing and Recovery
Post-surgical care is a vital aspect of successful recovery for patients undergoing surgery for hypospadias. Close attention to hygiene practices, wound care, and monitoring for any signs of infection or complications is necessary. Pediatric healthcare providers should provide comprehensive guidelines for post-surgical care, which may include recommendations for pain management, bathing practices, and activity restrictions.
Regular follow-up appointments are crucial for tracking the healing process, evaluating the surgical outcomes, and addressing potential long-term complications. Parents may also consider counseling support for emotional adaptations as their child grows and navigates the social implications tied to hypospadias.
Ultimately, a supportive, informed approach involving parents, healthcare providers, and mental health professionals can significantly enhance recovery outcomes and foster positive self-image and adaptation in childhood and beyond.
Living with Hypospadias: Long-Term Outlook and Considerations
Psychosocial Impact: Navigating Emotions and Relationships
The psychosocial implications of hypospadias can be profound and multifaceted. Psychological impacts may manifest early in life, as children with this condition might face challenges concerning body image, social interactions, and self-esteem. Beyond the physical treatment, comprehensive psychosocial support is vital for promoting adaptive coping strategies.
As children grow, they may become increasingly aware of their differences, and this knowledge can lead to anxiety or issues with peer relationships. Communicating openly about the condition at age-appropriate levels and encouraging dialogues about differences can foster a sense of acceptance and inclusivity. Involving mental health professionals in therapeutic contexts may further help children and their families gain tools to navigate these social complexities healthily.
Future Health Implications: What to Monitor Over Time
Long-term monitoring and follow-up for children treated for hypospadias are essential components of ongoing care. Regular evaluations by pediatric urologists ensure that any potential issues whether physical or psychological are identified and addressed early. In particular, experts will assess for urinary function, potential scarring, and any pubertal development concerns that may arise as the child matures. Awareness and vigilance for signs of complications, including urinary incontinence, sexual dysfunction later in life, or psychological distress, are paramount for optimal outcomes.
Continued education regarding the condition, its implications, and available support services can empower individuals to manage their health proactively, enhancing their quality of life over the long term.
Empowering Conversations: Educating Yourself and Others
Education plays a vital role in demystifying hypospadias and promoting awareness within broader communities. Healthcare providers, educators, and families must join forces to ensure that individuals affected by this condition feel supported and validated in their experiences. Sharing information about hypospadias can help reduce stigma and normalize conversations surrounding this congenital condition.
Furthermore, creating forums for discussions both online and offline can connect families and individuals coping with hypospadias, encouraging the sharing of experiences and coping strategies. Access to credible resources, support groups, and education can empower those affected, fostering a sense of community and enhancing overall well-being.
In conclusion, understanding and addressing hypospadias requires a comprehensive, multifaceted approach that engages healthcare systems, families, and communities. Through thorough education, timely interventions, and nurturing psychological support, we can pave the way for positive outcomes and enrich the lives of those living with this condition.